With age, bone health can become a major concern, especially for postmenopausal women and the elderly. Osteoporosis, a disease characterized by decreased bone mineral density and deterioration of bone microarchitecture, results from an imbalance between bone resorption and bone formation. This process leads to increased bone fragility and a higher risk of fractures, particularly in the hip, wrist, and spine.
In addition to deficiencies in calcium, magnesium, or vitamin D—nutrients essential for bone mineralization—several factors influence the pathophysiology of osteoporosis. In postmenopausal women, the decline in estrogen levels plays a central role, as these hormones normally regulate the activity of osteoclasts (cells responsible for bone resorption). Without estrogen, osteoclast activity becomes excessive, leading to accelerated bone loss.
A sedentary lifestyle, combined with low physical activity, exacerbates this phenomenon. Physical activity, particularly weight-bearing exercises such as walking or strength training, stimulates osteoblasts (cells responsible for bone formation) and supports bone density. Conversely, an inactive lifestyle reduces this stimulation, leaving bones vulnerable.
The nutritional and toxic environment also plays a crucial role. An imbalanced diet, low in essential nutrients and high in acidifying substances (such as salt or processed foods), can disrupt calcium balance by increasing urinary calcium losses. Moreover, chronic exposure to toxins, such as alcohol, tobacco, or certain pollutants, can interfere with bone metabolism by increasing oxidative stress and inhibiting osteoblast function.
Certain chronic diseases further aggravate the situation. Endocrine disorders, such as hyperthyroidism or Cushing’s syndrome, increase bone resorption through hormonal mechanisms. Gastrointestinal diseases, such as celiac disease or malabsorption syndromes, impair the absorption of essential nutrients needed to maintain bone health.
Why choose PHYSIOMANCE® Ostéo Gold ?
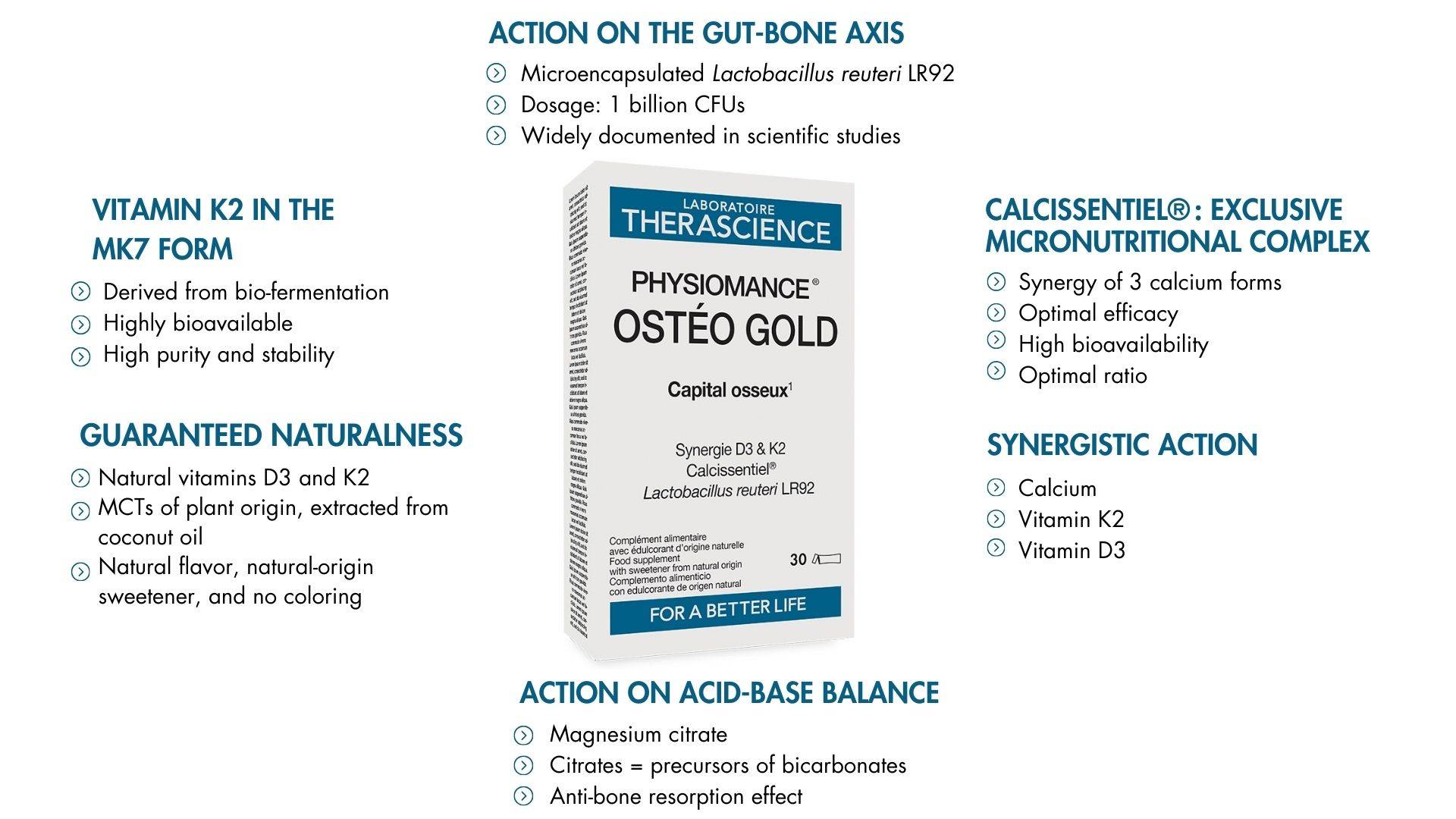
PHYSIOMANCE® Ostéo Gold stands out for its synergistic formulation, combining 5 carefully selected active ingredients known for their effectiveness. These ingredients are present in highly bioavailable forms, ensuring optimal absorption and ideal tolerance. PHYSIOMANCE® Ostéo Gold is a comprehensive and innovative choice to maintain bone density and support bone tissue structure.
PHYSIOMANCE® Ostéo Gold combines scientific advancements with carefully selected active ingredients to optimize bone health:
- - Calcissentiel® is an exclusive complex combining glycerophosphate, lactate, and calcium citrate. It is designed to optimize absorption and ensure maximum effectiveness. By combining the three best forms of calcium in an optimal ratio, we provide the most effective supplementation possible.
- - Magnesium in the form of citrate is distinguished by its exceptional bioavailability and its role in acid-base balance. This mineral plays a central role in bone mineralization, supporting essential enzymatic functions in bone matrix synthesis. Recent scientific advances have highlighted its importance in preventing deficiency-related fractures.
- -Vitamins D3 and K2, derived from natural sources, work in perfect synergy. Vitamin D3 facilitates intestinal calcium absorption, while vitamin K2, in its menaquinone-7 form, ensures calcium transport to the bones, preventing undesirable arterial accumulation. These coordinated mechanisms enhance both bone and cardiovascular health.
- - Finally, Lactobacillus reuteri LR92, a widely studied probiotic strain, plays a key role in maintaining intestinal microbiota balance. By improving the absorption of nutrients such as calcium and magnesium and reducing systemic inflammation, Lactobacillus reuteri LR92 contributes indirectly but significantly to preserving bone health.
What does science say?
According to the European Food Safety Authority (EFSA), the active ingredients selected in our PHYSIOMANCE OSTÉO GOLD complex are recognized for providing the following benefits :
- Contribute to the maintenance of normal bone structure (Calcium)
- Preserve bone density and strength (Calcium)
- Maintain optimal bone structure (Magnesium)
- Support the normal absorption of calcium and phosphorus (Vitamin D3)
- Help maintain normal bone structure (Vitamin D3 & K2)
- Contribute to reducing bone mineral density loss in postmenopausal women (Vitamin D3).
Lactobacillus reuteri LR92 faithas been the subject of numerous scientific studies, and its biological mechanism of action is well documented in the literature. Multiple studies highlight its interesting potential applications in health and prevention. However, to date, European legislation has not validated any health claims for Lactobacillus reuteri LR92. While no specific benefits are officially recognized, this probiotic strain is generating growing interest and presents promising opportunities that deserve further exploration.
Key benefits of PHYSIOMANCE® Ostéo Gold?
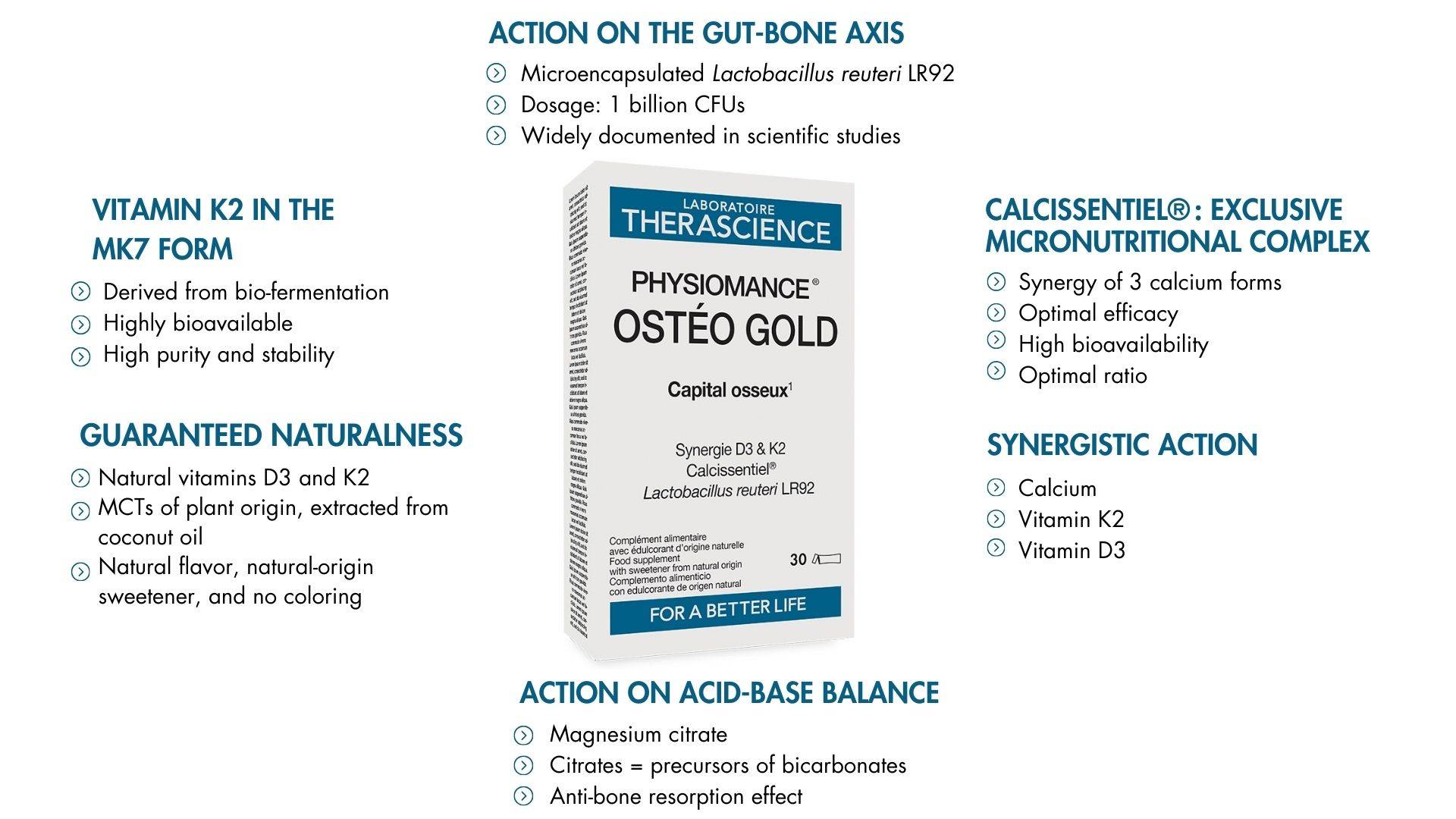
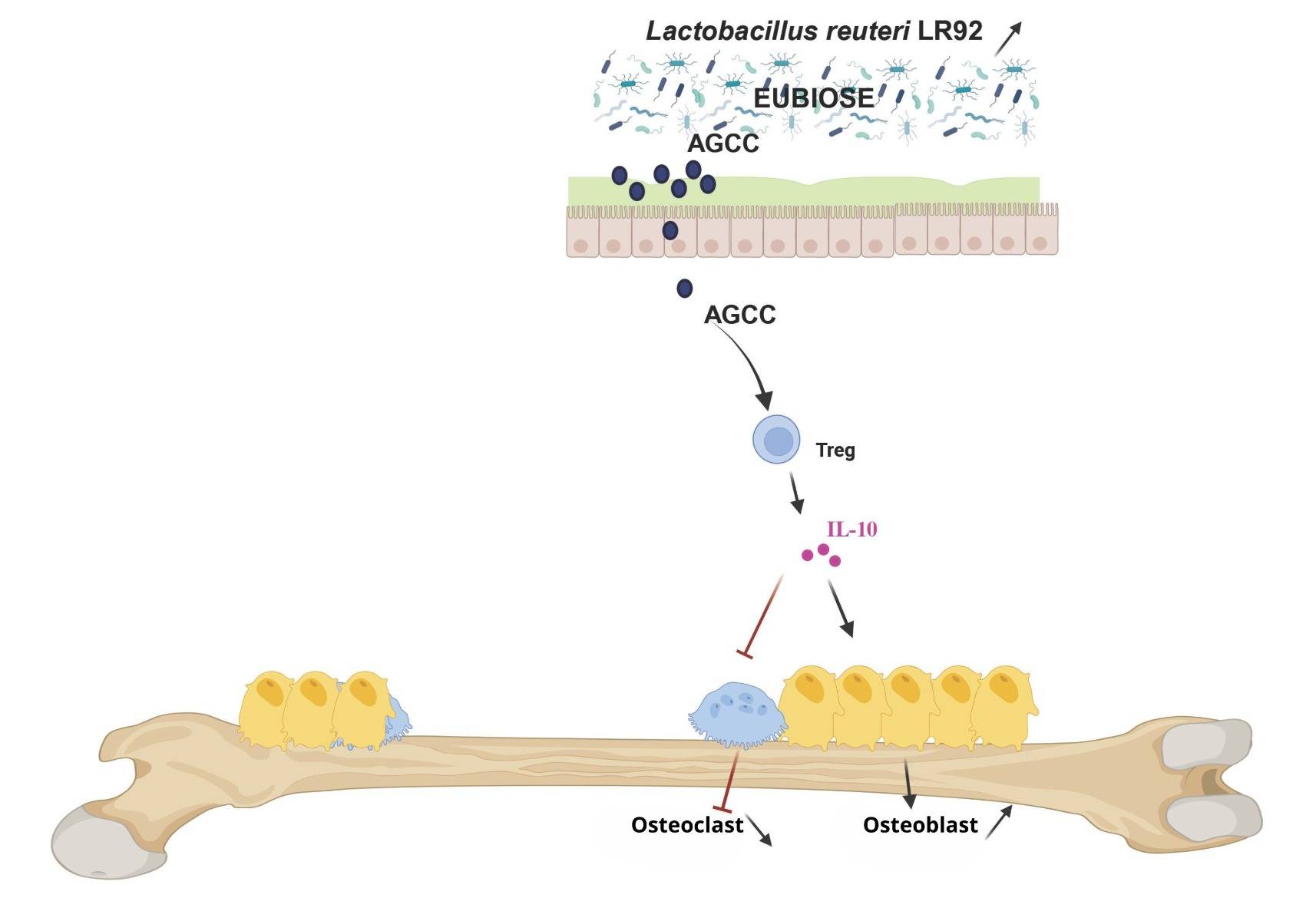
Action on the Gut-Bone Axis
Bone formation and resorption represent a dynamic balance essential to bone health. Osteoblasts, specialized cells, play a key role by forming bone through the deposition of bone matrix and promoting its mineralization.
Conversely, osteoclasts are responsible for the breakdown of old bone, a process called bone resorption, which releases calcium and phosphate into the bloodstream. This delicate balance between formation (performed by osteoblasts) and resorption (carried out by osteoclasts) is crucial for maintaining the strength, density, and integrity of bones. However, imbalances in this process can lead to pathologies. Excessive resorption results in conditions such as osteoporosis or bone fragility, while excessive formation can cause abnormal bone growth or rigidity.
The intestinal microbiota also plays a fundamental role in bone formation, influencing bone health through various mechanisms. It notably regulates nutrient absorption. For example, a balanced gut flora promotes the solubilization and absorption of calcium, a key mineral for bones, as well as vitamin D. Additionally, certain bacteria in the microbiota produce vitamin K2, which is essential for activating proteins involved in bone mineralization.
Calcissentiel® : Exclusive Micronutritional Complex
Calcium plays a key role in the mineralization and structure of the skeleton. It is the most abundant mineral in the body, accounting for 1.5 to 2% of our weight. Adequate calcium levels are essential for the normal functioning of the nervous system, muscle function, and the maintenance of normal bone structure.1Throughout life, total calcium mass tends to decrease, directly linked to bone density loss and alterations in microarchitecture, increasing the risk of fractures. The effectiveness of preventive supplementation depends on the form of calcium, which is why the THERASCIENCE Laboratory has developed an exclusive synergy of three organic calcium forms.
This patented formula, called Calcissentiel® comprises three calcium forms selected for their high bioavailability and excellent tolerance: lactate, glycerophosphate, and citrate, combined in an optimal ratio to ensure maximum effectiveness.
Calcium lactate is an excellent source of elemental calcium, offering high bioavailability and good tolerance. Calcium glycerophosphate was chosen for its high solubility and the benefits of its combination with phosphorus. The mineral phase of bone consists of hydroxyapatite [Ca₁₀(PO₄)₆(OH)₂], with a calcium-to-phosphorus ratio in bone of 7:1. Clinical data show that phosphorus enhances calcium retention and reduces urinary calcium excretion.2,3
Tricalcium citrate is known for its optimal absorption and its alkalizing effect. Citrates maintain the mineral-ionic balance and prevent bone demineralization by reducing urinary calcium excretion. Citrate intake has been shown to decrease markers of bone resorption.4 Calcissentiel® is an exclusive micronutritional complex that, through the combination of the best calcium forms in an optimal ratio, ensures good absorption and availability, guaranteeing excellent tolerance and maximum efficacy.
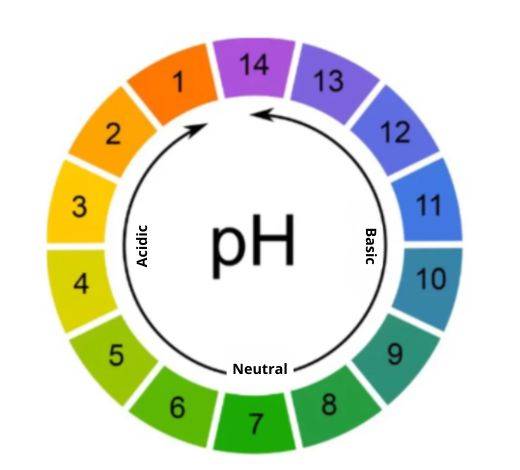
Action on Acid-Base Balance
The intake of magnesium citrates plays a crucial role in regulating the body's acid-base balance, which is directly linked to bone density loss.
A diet rich in animal proteins and low in fruits and vegetables can lead to an excess of acids in the body, disrupting the acid-base balance and causing mild but chronic metabolic acidosis. Citrates and bicarbonates act as bases capable of neutralizing this excess acidity. Once metabolized, citrates produce bicarbonate ions, which buffer hydrogen ions (H⁺) and help maintain a stable blood pH.
Furthermore, these substances play a key role in preserving bone health. In cases of acidosis, the body uses bones as a reserve of bases to neutralize acidity, leading to the loss of bone calcium, weakening bone structure, and reducing bone density. By providing citrates and bicarbonates through the diet, this harmful process can be avoided by directly neutralizing acids. Bicarbonates, in particular, reduce the activity of osteoclasts—the cells responsible for bone resorption—helping to preserve bone mass.
Lastly, citrates positively affect minerals essential for bones. By improving the intestinal absorption of calcium, they increase its bioavailability. This supports effective bone formation without excessively mobilizing the calcium reserves stored in bones.
Vitamin K2 in the MK7 form
To ensure optimal efficacy while maintaining maximum naturalness, we have selected an entirely natural vitamin K2, obtained through a specific and patented biofermentation process. This method allows us to offer a 100% plant-based vitamin, suitable for vegan diets and free from any allergens. Rigorous production results in a form of vitamin K2 MK7 with "trans" isomerism, the only biologically active form recognized by the body.
Vitamins K are distinguished by the variable length of their side chain, a key factor in their biological efficacy. While vitamin K1 (phylloquinone) has a fixed side chain, the various forms of vitamin K2 (menaquinones) have isoprenoid chains of varying length and saturation. The longer the side chain, the greater the biological efficacy. Among the forms of vitamin K2, menaquinone-7 (MK7) stands out for its superiority. Numerous clinical studies have demonstrated that MK7 has significantly higher biological activity than other forms of vitamin K, particularly menaquinone-4, whose shorter side chain limits its efficacy.
Vitamin K1, although primarily absorbed by the liver, is scarcely available for other tissues in the body. In contrast, vitamin K2 MK7, thanks to its unique structure, has an extended half-life. This means it remains active in the bloodstream for a prolonged period, allowing for more efficient use by various organs. Unlike vitamin K1, which is eliminated within 24 hours, vitamin K2 MK7 remains bioavailable for up to 72 hours after ingestion, ensuring three times higher absorption. Additionally, the serum concentration of menaquinone-7 after a meal is approximately 10 times higher than that of vitamin K1 and remains elevated for several days. This property helps improve overall vitamin status and maximizes its benefits for the body.
Guaranteed Naturalness
PHYSIOMANCE® Ostéo Gold has been meticulously formulated to address specific needs related to bone health while adhering to high naturalness standards. This supplement contains naturally sourced vitamins D3 and K2, two essential nutrients for maintaining normal bone structure and regulating calcium balance. Vitamin D3 plays a key role in calcium and phosphorus absorption, while vitamin K2 ensures the proper binding of these minerals to bones, contributing to their strength and resilience.
To ensure optimal powder quality, PHYSIOMANCE® Ostéo Gold includes plant-based medium-chain triglycerides (MCTs) extracted from coconut oil. These MCTs not only act as anti-caking agents but also enhance the stability and texture of the blends, providing a natural and healthy solution to the formulation.
Finally, PHYSIOMANCE® Ostéo Gold stands out for its commitment to naturalness, incorporating a natural flavor and a natural-origin sweetener to ensure a pleasant taste experience without the use of artificial additives. The absence of colorants reflects a respectful approach to health and product purity, perfectly aligning with the expectations of consumers demanding transparency and quality.
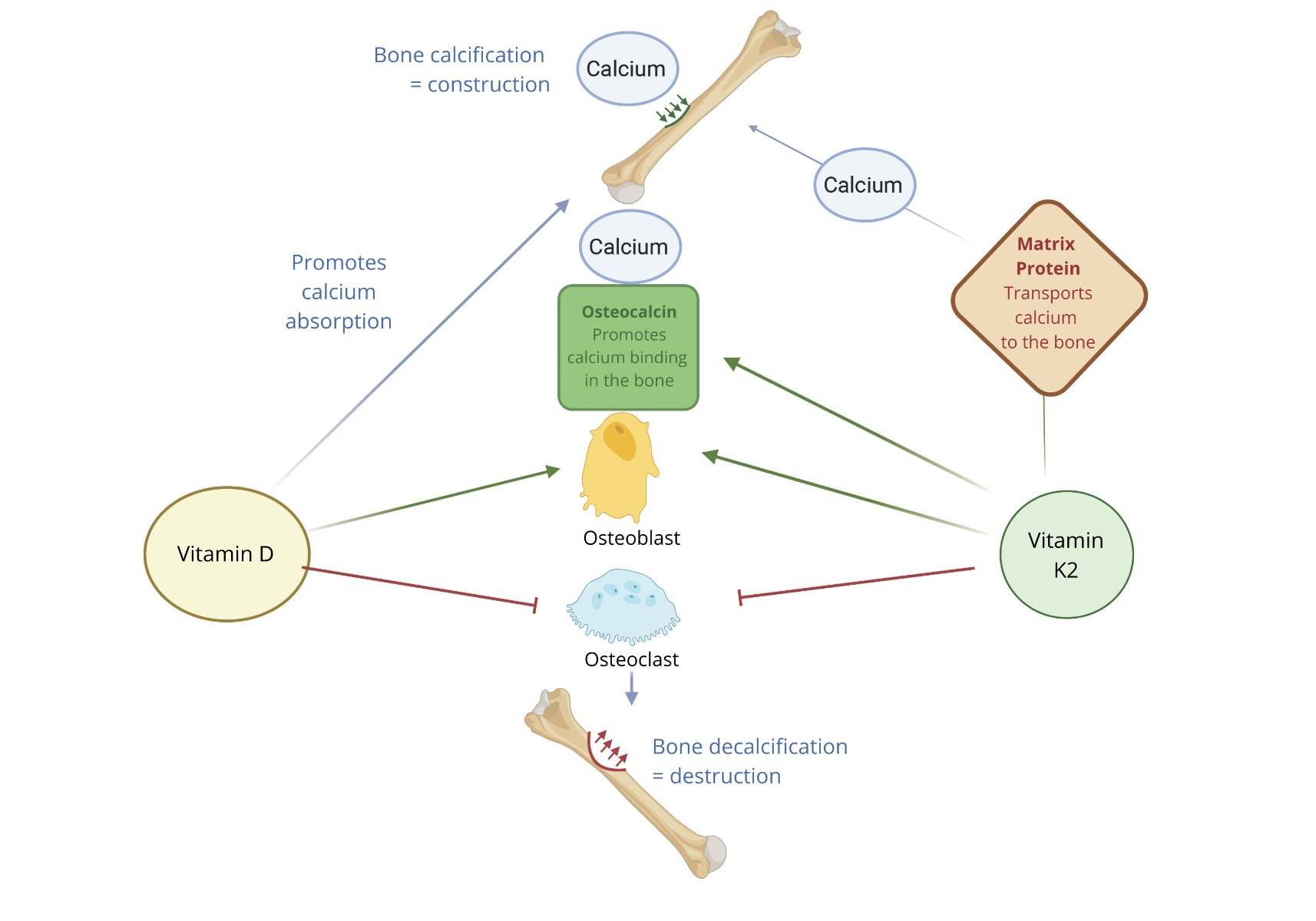
Synergistic Action
Calcium, vitamin K2, and vitamin D3 form an essential and interdependent triad to maintain good bone and cardiovascular health. Vitamin D3, or cholecalciferol, plays a central role in calcium metabolism by promoting its intestinal absorption. It increases the expression of calcium transporters, allowing calcium to enter the bloodstream. Once in circulation, vitamin D3 helps maintain optimal calcium levels by stimulating its reabsorption by the kidneys and regulating its utilization in bones, where calcium can be either released or stored depending on the body’s needs.
Vitamin K2, on the other hand, regulates calcium deposition by activating specific proteins. For example, it activates osteocalcin, a protein produced by osteoblasts, which allows calcium to integrate into the bone matrix, thereby strengthening the bones.
Additionally, vitamin K2 activates MGP (matrix Gla protein), a protein that prevents calcium deposition in soft tissues, such as arteries, thus reducing the risk of vascular calcification, a key factor in cardiovascular diseases. These two vitamins work in synergy to optimize calcium efficiency. While vitamin D3 increases calcium levels in the blood, vitamin K2 ensures that this calcium is properly utilized and directed to the bones. Without vitamin K2, the calcium provided by vitamin D3 could be misdirected and deposit in soft tissues or arteries, leading to calcification problems. Vitamin K2 ensures that calcium is used where it is needed while preventing undesirable deposits.
An imbalance in this intake can have consequences. For instance, supplementation with calcium and vitamin D3 without sufficient vitamin K2 may increase the risk of arterial calcification and cardiovascular disorders. Conversely, a deficiency in vitamin D3 may limit calcium absorption, even if vitamin K2 levels are adequate, which can weaken bones.
In summary, calcium provides the building blocks for bones, vitamin D3 enhances its absorption and availability in the bloodstream, and vitamin K2 acts as a regulator, directing calcium to the bones while preventing its accumulation in undesirable places such as the arteries. A balanced combination of these three elements is therefore essential to maintain bone health and cardiovascular well-being.