The painkiller ally
Pain
Pain is the leading cause of medical consultations and is defined as "an unpleasant sensory and emotional experience that may be associated with tissue damage". Pain is the subject of numerous clinical studies and fundamental research with the aim of understanding its mechanisms and evaluating the effectiveness of natural molecules to combat it. This is particularly the case with palmitoylethanolamide, also known as PEA.
Not one... but many pains
Pain can be classified into two categories: acute and chronic, which differ according to their duration.
Acute pain
Acute pain is a protective alarm signal. This signal is initiated by receptors called "nociceptors" located in the muscles, joints and skin and responding to different stimuli (temperature, burning, stinging, etc.). Other receptors, the chemoceptive receptors, are also specialised in the response to inflammatory molecules produced by immune cells, injured cells and nerve endings. The information is then transmitted along the nerves and spinal cord to the brain, which then interprets the message.
Chronic pain
When pain persists beyond 3 months, it becomes chronic. Considered a disease, chronic pain occurs in 30% of adults.1 It mainly affects the muscles and joints, and is also found in migraine headaches.
There are different categories of chronic pain: nociceptive, neuropathic, mixed or non disciplinary.
- Nociceptive pain is related to inflammation that lasts over time. It leads to chronic activation of the nerve fibres of the pain network and causes sensitisation of the nociceptors. This is known as excess nociceptive pain, which is characteristic of joint pain.
- Neuropathic painis caused by damage to the central or peripheral nervous system. This type of pain occurs, for example, after a cerebrovascular accident.
- Mixted pain, which can be found in cases of sciatica but also in cancer, is a combination of pain linked to excess nociception (due to inflammation) and neuropathic pain.
- Nociplastic pain is associated with the alteration of the pain detection system (nociception), in the absence of any injury. It corresponds to the modification of the pain control systems by the central nervous system, causing pain without apparent cause. Nociplastic pain is found in particular in patients suffering from chronic headaches or fibromyalgia.
The endocannabinoid system, a prime target for fighting pain
Within the body, the endocannabinoid system (ECS) modulates numerous physiological functions, in particular pain. Composed of receptors, enzymes and ligands, the ECS is activated by lipid molecules synthesised by the body: the endocannabinoids, of which the main representatives are anandamide (AEA) and 2 arachidonoylglycerol (2-AG).
Other endogenous molecules also activate the SEC. This is the case of palmitoylethanolamide (PEA), which gained fame thanks to the work published by the Nobel Prize winner for Medicine, the neurologist Rita Levi-Montalcini. Discovered in 1957 in egg yolk, the anti-inflammatory properties of PEA were soon described. PEA is also present in other foods (alfalfa sprouts, soya, corn, peanuts) but in very small quantities.
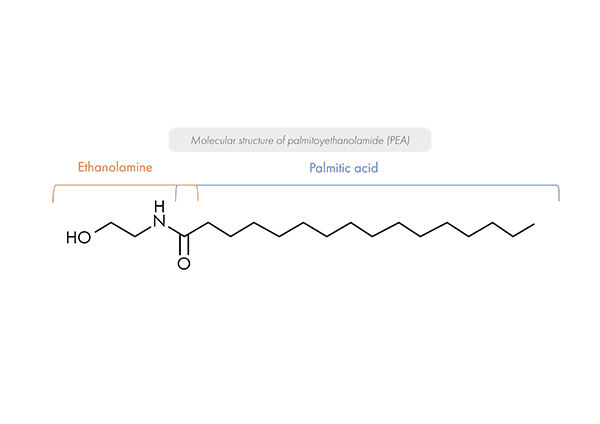 This fatty acid, which combines palmitic acid with an ethanolamine moiety, is naturally produced by the human body. It is found in almost all tissues, including muscle, heart and brain.2 The molecule is naturally synthesised by neurons, immune cells and microglia (brain immune cells).
This fatty acid, which combines palmitic acid with an ethanolamine moiety, is naturally produced by the human body. It is found in almost all tissues, including muscle, heart and brain.2 The molecule is naturally synthesised by neurons, immune cells and microglia (brain immune cells).
Because of its structural proximity to AEA, PEA is referred to as "endocannabinoid-like". However, although both molecules belong to the N-acylethanolamine family, they do not have the same mode of action.
While endocannabinoids and phyto-cannabinoids (such as CBD) bind directly to the main receptors of the ECS (CB1 and CB2), PEA acts indirectly on the body's ability to respond to the cannabinoids it produces naturally. By blocking the enzyme responsible for degrading endocannabinoids, PEA indirectly induces increased levels of AEA and 2-AG, prolonging their onset of action and inhibiting pain signal transmission. Although PEA production increases in pain, it decreases with age, thus reducing the endocannabinoid-like effect. In addition, PEA also decreases local inflammation by modulating the production of pro-inflammatory mediators.3 PEA is therefore particularly interesting for combating both acute and chronic pain, thanks to its anti-inflammatory and analgesic properties. It has the added advantage of being free of side effects and not inducing psychotropic effects. Thanks to its harmlessness, PEA is neither addictive nor does it induce drug interactions.4
The PEA of the THERASCIENCE Laboratory
With its concentrated formula providing 600 mg for 4 capsules of bioassimilable palmitoylethanolamide, PHYSIOMANCE PEA BIOASSIM from Laboratoire THERASCIENCE constitutes a nutritional support in case of pain, whether it is acute, chronic, neuropathic or inflammatory.
THERASCIENCE Laboratory has selected the PEA Levagen®+, associated with the LipiSperse® technological process in order to improve the bioavailability of PEA. Indeed, due to its hydrophobic nature, PEA is generally not very soluble in water, which explains its reduced effectiveness. The PEA Levagen®+ present in PHYSIOMANCE PEA BIOASSIM ensures the dispersion of PEA in the stomach, thus guaranteeing its optimal absorption by the body thanks to its bioavailability and high quality. 5
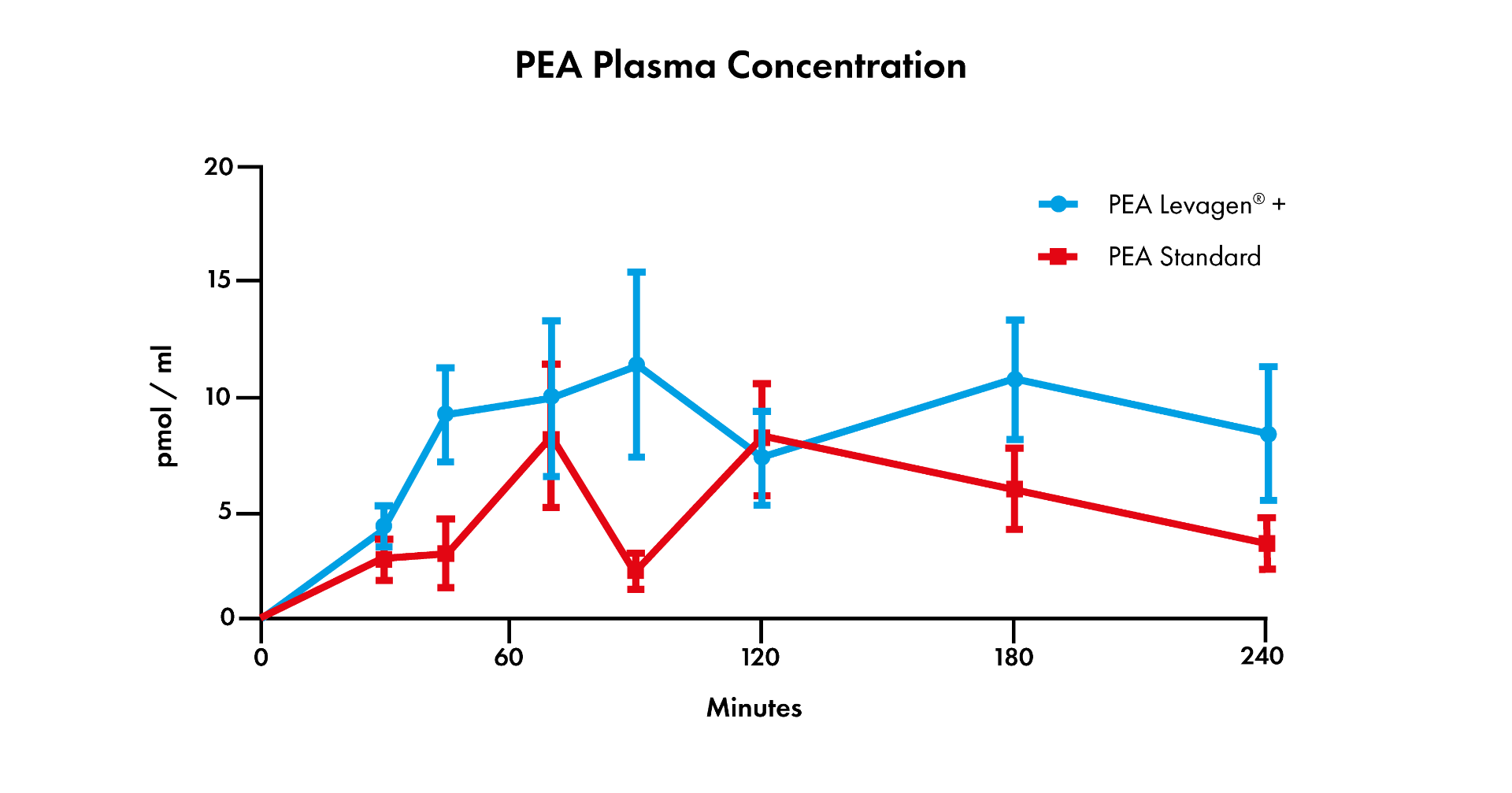
Its efficacy was demonstrated in a double-blind clinical study of 28 patients over 24 hours, where half of the participants received 300 mg of Levagen®+ PEA, while the other half received the same amount of PEA, but this time of standard quality. In sum, taking Levagen®+ PEA increases the plasma concentration of PEA by 1.75 times compared to standard PEA, thus ensuring the efficacy of our Levagen®+ PEA at lower concentrations than the standard forms.6
Bibliography
- Treede, Rolf-Detlef et al. “Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11).” Painvol. 160,1 (2019): 19-27.
- Gabrielsson, Linda et al. “Palmitoylethanolamide for the treatment of pain: pharmacokinetics, safety and efficacy.” British journal of clinical pharmacologyvol. 82,4 (2016): 932-42.
- Petrosino S, Di Marzo V. The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations. Br J Pharmacol. (2017);174(11):1349-1365.
- Artukoglu, Bekir Berker et al. Efficacy of Palmitoylethanolamide for Pain: A Meta-Analysis. Pain physicianvol. 20,5 (2017): 353-362.
- Briskey, D et al. “Increased bioavailability of curcumin using a novel dispersion technology system (LipiSperse®).” European journal of nutritionvol. 58,5 (2019): 2087-2097.
- LIPISPERSEa (2019). Advanced dispersion technology.